How processing your trauma can reduce pain and inflammation
Sep 12
/
Dr Sula Windgassen
As a health psychologist specialising in the mind-body connection, I've witnessed both first and second hand reductions in chronic pain after processing past trauma. But this isn't just anecdotal - there's compelling research showing how unprocessed trauma can literally rewire our pain processing systems, keeping us stuck in cycles of chronic pain and inflammation.
What's fascinating is that trauma doesn't just live in our minds - it creates measurable changes in our nervous system, immune function, and even how our spinal cord processes pain signals. The good news? These changes aren't permanent. When we process past trauma, we can literally help our brains recalculate pain, often leading to profound reductions in symptoms that may have persisted for years.
Can processing my trauma reduce pain and inflammation?
My first experience of the trauma therapy eye-movement desensitisation and reprocessing (EMDR) was when I was training to be an EMDR therapist. During the training practice I found myself transported back to my childhood home, milliseconds equating to whole years of lived experience, as my brain rapidly considered and contextualised things. I found myself recognising realities I could never have consciously conjured. The recognition of which made me feel much different. Lighter, freer, less oppressed. It was a revelation – the whole experience.
In the following days I was sceptical. Surely, I'll start feeling the same old way again about the same little triggers. And yet I didn't. I felt detached, but positively so. More objective and unaffected. These were things that for years had really hung around.
Then later, in the midst of the COVID-19 pandemic, I realised I was burnout and my burnout was reducing my tolerance for the same past wounds, so I sought out an EMDR therapist. I found it similarly transformative. This time, it wasn't a one-off, there was space to explore the many and various interconnections of the past and how that had shaped my self-concept, my feelings and even my health.
A lot was processed and a lot changed, but the sense that sticks with me to this day, is the physicality. I was not focussing on health stuff, and yet I felt lighter, less clogged and I felt more present. By this point in my own therapy, I'd been using EMDR a lot with my NHS patients with chronic illness and I'd been seeing significant shifts in their functioning, in their mood state and even in their symptoms. But how could this be?
Trauma, stress and hormones, immune function and inflammation
If you're a long-time newsletter subscriber or you have read the previous blogs, you'll be familiar with the effects of stress and trauma on the brain, the nervous system and the immune system. In a nutshell, it is well-established that your brain processing and even structure can be changed by chronic or extreme stress and these changes lead to changes in how your nervous system works, how your neuroendocrine (hormonal) systems work and what is happening in your immune system (1–3). There are so many complexities in this inter-tangled web of communication systems, but what we can clearly observe, is that these changes also change sensory experiences including pain.
Why you feel pain
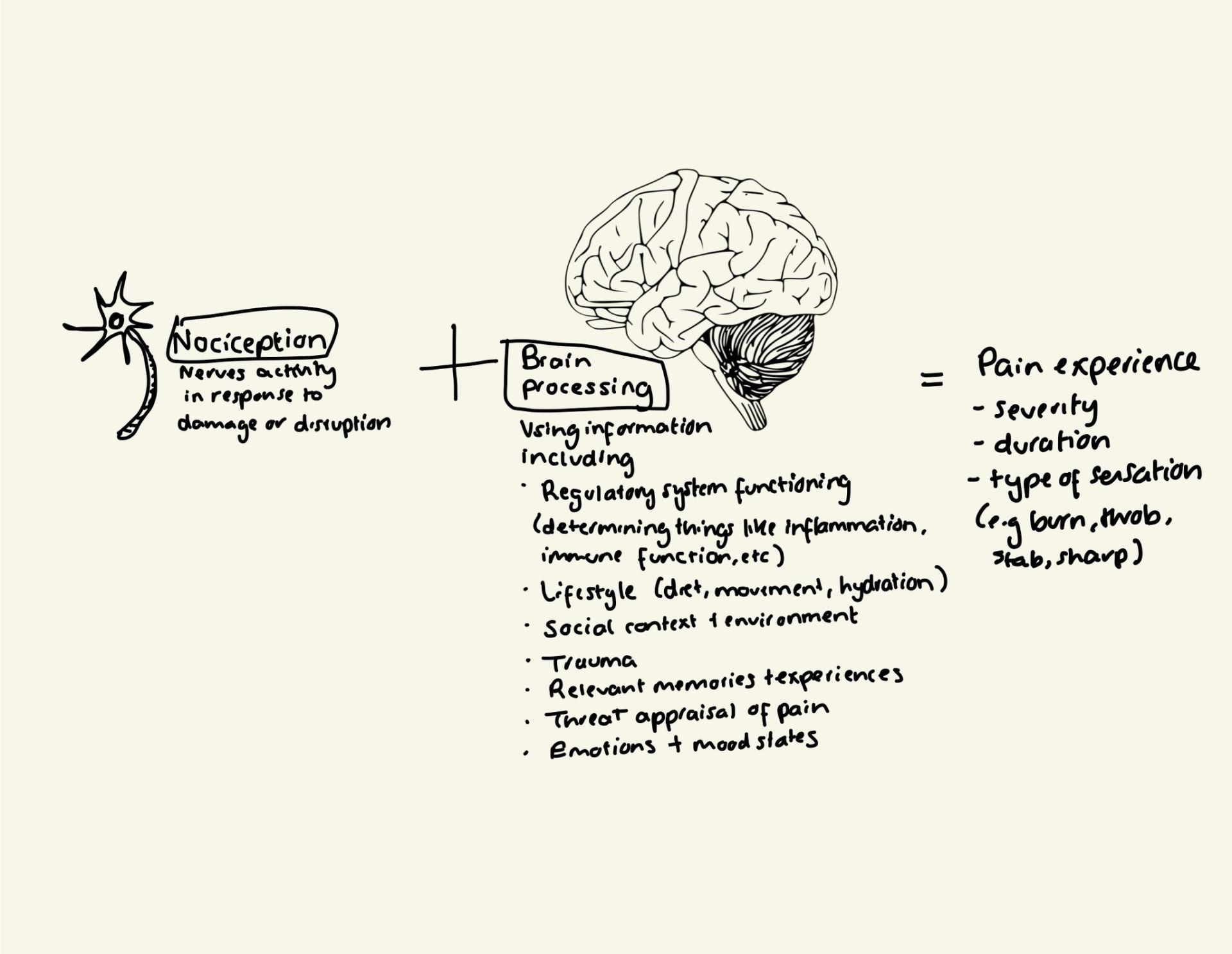
Pain is the combination (generally) of two broad things: signalling from nerves at the site of pain and calculations made in the brain. This is the pain equation. However, research has shown that sometimes the brain keeps calculating pain long after the nerves are firing (4). This is why injury can result in chronic pain, even once the injury is healed. There are lots of names for this type of pain including neuroplastic pain, or neuropathic pain. The fault in the brain calculation is often due to multiple strands of 'data' clouding clarity in the brain. Data such as emotion; how much threat your brain is detecting based on emotion and threat processing centres in the brain like the amygdala, but also based on how your autonomic nervous system is generally behaving (4,5). Erratic responses and dysregulation can prime the brain to amplify pain (1).
To summarise, you can feel physical pain whether or not there is damage to tissue, based on what is happening in your brain. The more threatening stuff happening there (high stress, traumatic experiences unprocessed, emotion dysregulation) the more likely the brain is to miscalculate and amplify or maintain pain where there shouldn't be any.
How chronic or extreme stress worsens pain or keeps it going
Previously I've written about some of the ways chronic or extreme stress changes your neurobiology, changing brain activity, changing hormonal balances, releasing and later suppressing cortisol, affecting nervous system activity. Well, all of those changes, can impact how pain is processed. In one fascinating animal study (which has its place in understanding neurobiology), researchers found that chronic stress caused inflammation in the spinal cord, making nerves residing there 'jumpy' making the animals more sensitive to touch and pain (1). In the same study they found that this stress contributed to anxiety, which didn't impact the spinal inflammation but amplified the sensory experience of pain, making it last longer and feel more severe. Previous studies demonstrating overlaps in where the brain processes pain and emotion can go some way to explain this physical change in pain (6).
The pain is not caused by anxiety but amplified by it – physiologically. The pain is real – changed by neurobiological shifts in the body. This study demonstrates but one pathway of pain processing being changed. The spinal cord projects out through 31 pairs of nerves to the rest of the body via the peripheral nervous system, so activity here can have a big impact on pain and sensation in the body. The spinal cord is the mediating highway between body and brain.
Other studies have shown that chronic stress and trauma can fundamentally change the body's own internal system that produces chemicals we need to balance mood, regulate stress and control pain – the internal opioid system (7). The more disrupted by stress this system is, the less able the body naturally is to regulate pain signals, leading to increased pain sensitivity.
Past trauma as a stressor (that can be processed)
When you experience trauma, your brain's ability to contextualise those memories and regulate the emotional impact, is disrupted (8). That means that the experience can sit in the periphery, out of consciousness, yet still affecting your mood and how you feel day to day. This is reflected in the comments I hear from people after EMDR processing, talking about feeling like a weight has been lifted, or things feel clearer or brighter. Your brain has had the opportunity to consolidate a lot of messy, threatening stuff that has been splattered all of your emotion, sensory and cognitive processing regions of the brain. When you process the past, it can alleviate a huge emotional burden, improving emotion regulation and alleviating a lot of ongoing stress (9). Studies have shown changed default emotion brain circuitry after the trauma processing therapy, EMDR (10).
This can potentially help reduce pain, in the same way that increasing stress and anxiety worsens pain – you are down amplifying the switch, helping your brain turn down the volume on pain.
Fascinatingly, there may be other mechanisms that explain how processing past trauma -especially past traumatic experiences of pain or symptoms – can reduce pain. This relates to the concept of the brain 'calculating' pain, using various different data points including previous experiences with pain. When you help the brain differentiate past traumatic pain memories from the present, it may stop it from factoring these into the 'pain calculations'. If the threatening context and appraisals of pain are massively reduced because of this process, the brain can update its calculations, down-regulating or even extinguishing pain (4,9).
I've seen this effect with my own eyes. And it is also reflected in the research.
Evidence of processing trauma, changing pain and inflammation
Eye movement desensitisation and reprocessing (EMDR) is a therapeutic process originally developed for trauma in the context of PTSD. However, since its origin it has been adapted and studied in a variety of contexts including chronic pain. Although research is still in its infancy to some degree, the results are compelling.
Studies have shown that EMDR can significantly reduce pain in the context of cancer recovery (11) and in inflammatory conditions like rheumatoid arthritis (12). Studies have shown really startling results, with 86% of patients with phantom limb pain reporting complete or almost complete pain recovery and other studies demonstrating drastic improvements in back pain (13).
We have a way to go, before we can with certainty isolate mechanisms that change from trauma processing. But certainly so far we know that memory consolidation in the hippocampus and downregulation of emotional circuitry play a role (10). Broadly speaking, research demonstrates that working with psychological processes related to illness also helps to reduce inflammation, so potentially these processes work from the 'body-up' to the brain as well as from the brain down to the body (14).
As ever… I have a billion and one tabs open with fascinating research, but I'll fight the urge to try and cover everything and hope this gives you a good idea of how much scope there is for working with your body.
TLDR
The bottom line: Unprocessed trauma creates ongoing stress in your nervous system that can amplify pain signals and maintain inflammation - even when there's no current tissue damage. Research shows trauma therapy like EMDR can significantly reduce chronic pain by helping your brain differentiate between past threatening experiences and present reality. Studies demonstrate up to 86% complete pain recovery in some conditions, with measurable changes in brain circuitry after trauma processing. Your pain is real, but trauma processing offers a evidence-based pathway to help your brain turn down the volume.
References:
1. Rivat C, Becker C, Blugeot A, Zeau B, Mauborgne A, Pohl M, et al. Chronic stress induces transient spinal neuroinflammation, triggering sensory hypersensitivity and long-lasting anxiety-induced hyperalgesia. PAIN. 2010 Aug 1;150(2):358–68.
1. Rivat C, Becker C, Blugeot A, Zeau B, Mauborgne A, Pohl M, et al. Chronic stress induces transient spinal neuroinflammation, triggering sensory hypersensitivity and long-lasting anxiety-induced hyperalgesia. PAIN. 2010 Aug 1;150(2):358–68.
2. Lenart-Bugla M, Szcześniak D, Bugla B, Kowalski K, Niwa S, Rymaszewska J, et al. The association between allostatic load and brain: A systematic review. Psychoneuroendocrinology. 2022 Nov 1;145:105917.
3. Finlay S, Roth C, Zimsen T, Bridson TL, Sarnyai Z, McDermott B. Adverse childhood experiences and allostatic load: A systematic review. Neuroscience & Biobehavioral Reviews. 2022 May 1;136:104605.
4. Apkarian AV, Hashmi JA, Baliki MN. Pain and the brain: Specificity and plasticity of the brain in clinical chronic pain. PAIN. 2011 Mar 1;152(3, Supplement):S49–64.
5. Xanthos DN, Sandkühler J. Neurogenic neuroinflammation: inflammatory CNS reactions in response to neuronal activity. Nat Rev Neurosci. 2014 Jan;15(1):43–53.
6. Malfliet A, Coppieters I, Van Wilgen P, Kregel J, De Pauw R, Dolphens M, et al. Brain changes associated with cognitive and emotional factors in chronic pain: A systematic review. European Journal of Pain. 2017;21(5):769–86.
7. Nakamoto K, Tokuyama S. Stress-Induced Changes in the Endogenous Opioid System Cause Dysfunction of Pain and Emotion Regulation. International Journal of Molecular Sciences. 2023 Jan;24(14):11713.
8. Del Casale A, Ferracuti S, Barbetti AS, Bargagna P, Zega P, Iannuccelli A, et al. Grey Matter Volume Reductions of the Left Hippocampus and Amygdala in PTSD: A Coordinate-Based Meta-Analysis of Magnetic Resonance Imaging Studies. Neuropsychobiology. 2022 Feb 14;81(4):257–64.
9. Johnson BN, McKernan LC, Bruehl S. A Theoretical Endogenous Opioid Neurobiological Framework for Co-occurring Pain, Trauma, and Non-suicidal Self-injury. Curr Pain Headache Rep. 2022 June 1;26(6):405–14.
10. Rousseau PF, El Khoury-Malhame M, Reynaud E, Zendjidjian X, Samuelian JC, Khalfa S. Neurobiological correlates of EMDR therapy effect in PTSD. European Journal of Trauma & Dissociation. 2019 May 1;3(2):103–11.
11. Abdi N, Malekzadeh M, Fereidouni Z, Behnammoghadam M, Zaj P, Mozaffari MA, et al. Efficacy of EMDR Therapy on the Pain Intensity and Subjective Distress of Cancer Patients. Journal of EMDR Practice and Research. 2021 Feb;15(1):18–28.
12. Nia NG, Afrasiabifar A, Behnammoghadam M. Comparing the effect of eye movement desensitization and reprocessing (EMDR) with guided imagery on pain severity in patients with rheumatoid arthritis. Journal of Pain Research. 2018 Sept 28;11:2107–13.
13. Tesarz J, Wicking M, Bernardy K, Seidler GH. EMDR Therapy's Efficacy in the Treatment of Pain. Journal of EMDR Practice and Research. 2019 Nov;13(4):337–44.
14. Seaton N, Hudson J, Harding S, Norton S, Mondelli V, Jones ASK, et al. Do interventions for mood improve inflammatory biomarkers in inflammatory bowel disease?: a systematic review and meta-analysis. eBioMedicine [Internet]. 2024 Feb 1 [cited 2025 July 16];100. Available from: https://www.thelancet.com/journals/ebiom/article/PIIS2352-3964(23)00476-0/fulltext?ref=dissidentmd.com
About Dr Sula Windgassen, PhD
Dr Sula is a Health Psychologist, Cognitive Behavioural Therapist, Eye Movement Desensitisation & Reprocessing (EMDR) Therapist and Mindfulness Teacher. Trained at King's College London & publishing papers on the use of psychology to improve health and whole-person wellbeing.
Featured links
Copyright © 2026