Does trauma cause health issues or do health issues cause trauma?
Sep 5
/
Dr. Sula Windgassen
If you've ever wondered whether your difficult life experiences could be connected to your health struggles, you're not alone.
Many people with chronic conditions question this link, often dismissing their past as "just life" or insisting their trauma happened too long ago to matter now. Yet research reveals a compelling story about how our minds and bodies are far more interconnected than we might expect. Understanding this connection isn't about blame or oversimplification - it's about recognising the complex ways that biology and psychology work together, and importantly, how this knowledge can empower your healing journey.
Trauma and chronic illness or health issues
Over the years I've spoken to many people who have shyly told me that they didn't think they had trauma, but do think that they've had major stress that may have impacted on their health. Others have told me definitively their childhood stress or trauma has absolutely nothing to do with their health – and I should add, sometimes it doesn't. I myself, when I got ill with bladder symptoms that seemingly had 'no cause' vehemently rejected any connection with trauma.
There can be an incredulity that what we conceptualise in our minds as 'just life experiences' can infiltrate our biology. So, what does the research say?
Stress or trauma?
I've previously written about the definition of trauma, differentiating it from adversity and chronic stress. When making this distinction, I've also emphasised that biologically they both are on the same continuum with extreme trauma at the extreme end of the spectrum and adversity a little further down. What this spectrum doesn't take into account is time-span. Little drips of the same poison over time can culminate in similar effects to one big dose of poison all-in-one.
As I consider the science with you now, I'm including research that looks at adversity and trauma, which are often grouped together in research assessing childhood experiences.
Childhood adversity and trauma increases your risk of chronic illness
The research is pretty definitive on this one and shows a dose-dependent relationship. The more adversity or trauma you experienced (which may equate to more extreme, different types of adversity or trauma, or frequency or length of experience of trauma), the more likely you are to develop a chronic illness(1,2).
A common measure of childhood adversity is the Adverse Childhood Experience Questionnaire (ACEs), which captures traumatic childhood experiences as well as chronic childhood stressors. The higher the ACE score, the more likely you are to develop a chronic illness, with research suggesting a cut-off ACE score of 4, meaning that if you an ACE score of 4 or more, you are significantly more likely to develop a chronic illness (1).
You may be surprised both at what constitutes and ACE and therefore at what your own ACE score is.
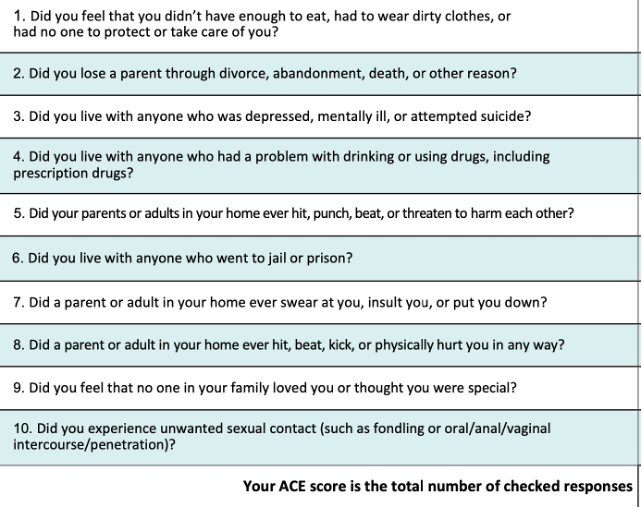
Items 3, 4, 7, 9 are experiences that many a person shrugs off 'that's just how it was' , minimising the impact because they haven't ever had it acknowledged as something significant. Even with the other items depicting physical abuse or threat to safety, it can be common for peoples' brains to have also found some way to minimise, which can be very protective, as well as prohibitive of healing.
The statistics can be quite mind-blowing on this one.
One study found that childhood trauma increased the odds of developing chronic fatigue syndrome by 500% (6 fold increase) (3). Along with sexual abuse, emotional abuse and neglect were the types of trauma that significantly differentiated those with CFS from their study counterparts. Not being tended to when upset, being told you are embarrassing or making problems for the grown-ups, being ignored or cold-shouldered, are all examples of the sorts of experiences that constitute these risk factors. Again, these are things that are often dismissed as 'that's just how it was at home' or 'my parents had their own stuff' or 'it wasn't bad compared to…'
In a study of university students, researchers found that childhood trauma was significantly associated with chronic pain including chronic headache, back pain and dysmenorrhea (4). In a meta-analysis (study pooling results from multiple studies), researchers showed a small but definitive link between childhood abuse and neglect and the later development of autoimmune diseases (5). Other studies show similar patterns of childhood adversity predicting gut conditions (6), pelvic conditions (7) and inflammatory conditions (8).
Trauma and stress as an adult – can it trigger illness?
Again we've got more definitives from the research here. Research shows that one-off extreme instances of trauma like in the context of PTSD can make it more likely for you to develop health issues (9,10). Research also shows that experiencing ongoing, cumulating stress also makes the development of a chronic illness more likely (11,12).
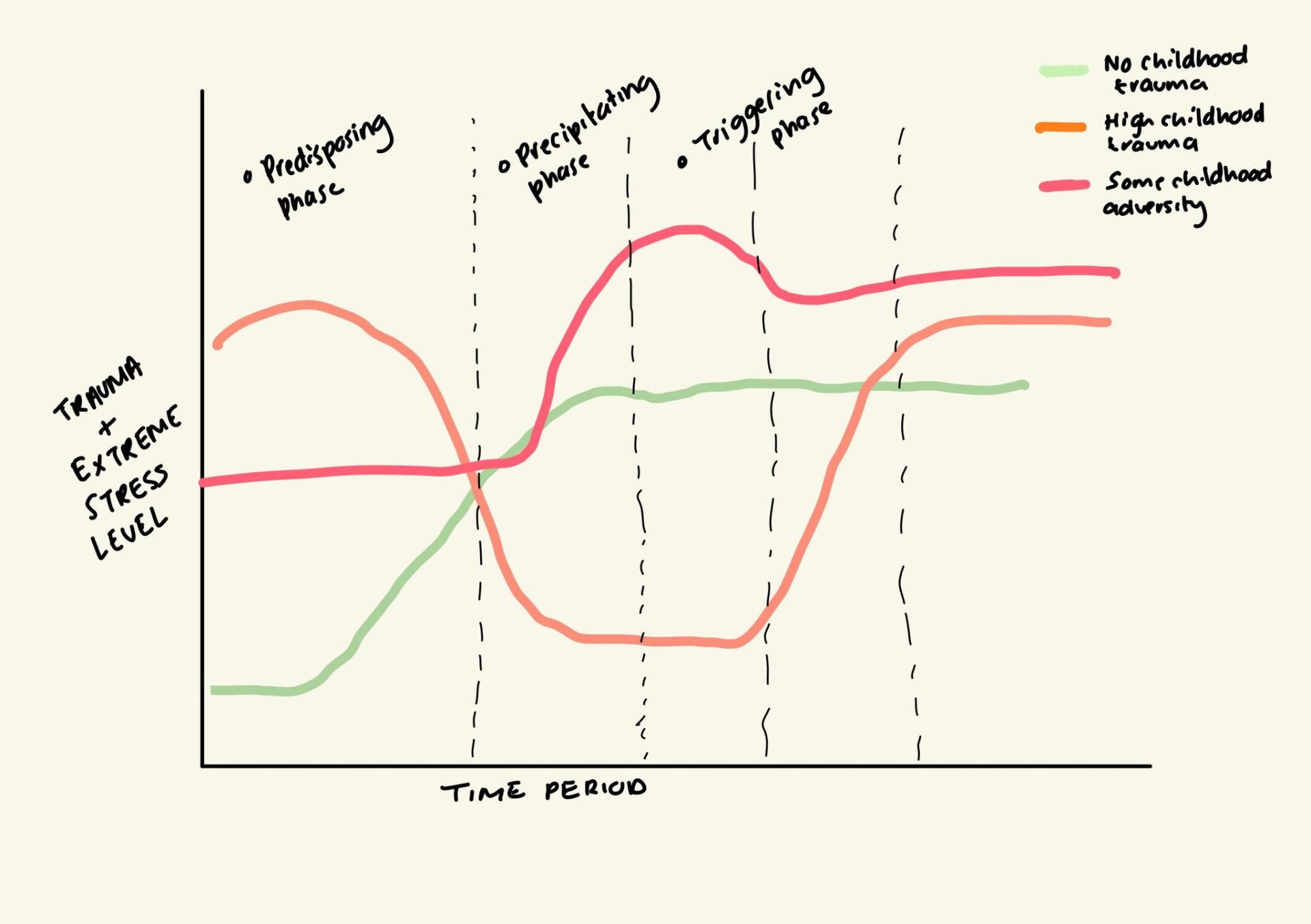
Here the word 'trigger' is important. People often assume this means you have a stressful experience or trauma and then that flips a switch and your health changes. This assumption is the reason why people don't readily identify with the idea that their health issues have any relationship with their life experiences.
“It's always been stressful, so why would this start now?”
Or “yes that did happen to me, but that was months ago and I was fine since, so this can't be related!”
The timescales of the body are often not the timescales that make sense to you. Under your consciousness every cell of your body is going through transformation, some quick, others slower. Transformation in one bunch of cells can gradually start to impact another bunch until your conscious experiences starts to feel a lot different.
Trauma and chronic stress can trigger illness or health issues; it just might not be as instantaneous as you think.
“I wasn't stressed until I got ill”
In therapy with 100s if not 1000s of people now, I've heard trajectories of stress and health and how they cooccur and shape each other. Another reason that you might not readily identify with the idea that stress or trauma had a role to play in the onset of your illness, is because in contrast to getting ill, your life was not stressful at all! You were cruising through doing life without much concern and doing what you needed to do. The most notable trauma being when you started experiencing health issues. I hear you.
I want to be clear, not everyone with chronic illness or health issues has experienced trauma and perhaps may not have had hugely elevated stress. This is part of a biopsychosocial approach to health – there is a lot of variation. And the combination of factors that combine to cause health issues for one person, won't be the same as for another. So it can be entirely true that it was the health issues that elevated the stress or constituted the trauma.
The trauma of health issues
I previously defined trauma, as is used to conceptualise the diagnosis of post traumatic stress disorder (PTSD), as 'exposure to actual or threatened death, serious injury, or sexual violence'. When people have health issues, there is lots of exposure to actual or threatened serious injury (or harm, which is used interchangeably in this definition of trauma), just by the experience of symptoms. Pain is an experience of harm. Add to that the appraisals we might have if that pain is unexplained like 'something really bad is happening in my body' or 'this could be a sign of a serious illness that will get worse', all brain processes are those of high-threat and alarm. In the context of other illnesses, where the aetiology is known, the threat may be just as great or greater. For example, in endometriosis where there may be sorely inflamed lesions, or in inflammatory bowel disease where there may be tissue degradation, these bodily changes would classify as injury or harm. Just because there is no external force or perpetrator, doesn't make it less traumatic.
The research water is a little muddied and unclear when it comes to conceptualising elements of chronic illness or health events as traumatic, although many conceptualisations of chronic stress and stressful life events do recognise illness as a major stressor (13,14). What I conceptualise with my clients, and members of Body Mind Connect, is that the experience of ill-health itself can be a major stressor and itself make you more likely to experience trauma. Completely uncontrollable flare ups, medical trauma, abandonment in relationships, all of these can classify as trauma or extreme stress, and all of these are more likely and common when you have a chronic illness or health issues.
Understandably therefore it can feel like you are drowning in quicksand as you are told 'stress is bad for your health' while your health causes you a lot of stress. This is why a biopsychosocial approach to health is so important. It allows you to consider the interrelationship between your biology and your psychology and how both are constantly impacting each other, and where there is scope for changing that conversation. It is not about positive thinking or denying your stress, it is actually about learning new ways to inhabit and work with that stress, so the stress itself (and your body) becomes less of a stressor. This might sound like a bit of a riddle and that's because it isn't intuitive necessarily. Having a framework that can guide you how to change your relationship with your body when it is unruly and stress when it is unrelenting, can fundamentally make your body feel safer.
In case you haven't got it,here is a link to my 30page workbook on chronic stress and illness that gives you an idea on this framework and all the many and varied strategies within it.
In case you haven't got it,here is a link to my 30page workbook on chronic stress and illness that gives you an idea on this framework and all the many and varied strategies within it.
TLDR
Childhood trauma dramatically increases your risk of chronic illness: The research is definitive - adverse childhood experiences create a dose-dependent relationship with disease risk, with ACE scores of 4+ significantly increasing your likelihood of developing chronic conditions
Adult stress and trauma can trigger illness, but not always immediately: Your body operates on different timescales - cellular transformation happens gradually, so the connection between stressful events and health changes might not be obvious or instant
Health issues themselves become traumatic experiences: Chronic symptoms create ongoing threat signals - unexplained pain, uncontrollable flare-ups, and medical trauma all register as harm to your nervous system, creating new stress
You can feel trapped in a stress-illness cycle: Being told "stress is bad for your health" while your health causes stress - this creates a frustrating loop where the very thing harming you (stress) is caused by the thing you're trying to heal (your illness)
It's not about positive thinking or blame: A biopsychosocial approach recognises the constant conversation between your biology and psychology, showing where you can intervene to change that dialogue
The key insight: Trauma and stress don't just "cause" illness in a simple cause-and-effect way - they create complex, ongoing interactions between your mind and body that can perpetuate suffering.
Bottom line: Understanding how stress, trauma and illness feed into each other isn't about finding fault - it's about learning new ways to work with your body and stress so your entire system feels safer, breaking the cycle that keeps you stuck.
Empty space, drag to resize
References
1. Senaratne DNS, Thakkar B, Smith BH, Hales TG, Marryat L, Colvin LA. The impact of adverse childhood experiences on multimorbidity: a systematic review and meta-analysis. BMC Med. 2024 Aug 15;22(1):315.
2. Alhowaymel FM, Kalmakis KA, Chiodo LM, Kent NM, Almuneef M. Adverse Childhood Experiences and Chronic Diseases: Identifying a Cut-Point for ACE Scores. International Journal of Environmental Research and Public Health. 2023 Jan;20(2):1651.
3. Heim C, Nater UM, Maloney E, Boneva R, Jones JF, Reeves WC. Childhood Trauma and Risk for Chronic Fatigue Syndrome: Association With Neuroendocrine Dysfunction. Archives of General Psychiatry. 2009 Jan 1;66(1):72–80.
4. You DS, Albu S, Lisenbardt H, Meagher MW. Cumulative Childhood Adversity as a Risk Factor for Common Chronic Pain Conditions in Young Adults. Pain Medicine. 2019 Mar 1;20(3):486–94.
5. Jesuthasan J, Watson CJ, Hafeez D, Lynch-Kelly K, Danese A, Pollak TA. Childhood adversity as a risk factor for autoimmune disease: A systematic review and meta-analysis with implications for psychiatry. Brain, Behavior, and Immunity. 2025 Aug 1;128:643–53.
6. Wiley JW, Higgins GA. Epigenomics and the Brain-gut Axis: Impact of Adverse Childhood Experiences and Therapeutic Challenges. J Transl Gastroenterol. 2024 June;2(2):125–30.
7. Krantz TE, Andrews N, Petersen TR, Dunivan GC, Montoya M, Swanson N, et al. Adverse Childhood Experiences Among Gynecology Patients With Chronic Pelvic Pain. Obstetrics & Gynecology. 2019 Nov;134(5):1087.
8. Furman D, Campisi J, Verdin E, Carrera-Bastos P, Targ S, Franceschi C, et al. Chronic inflammation in the etiology of disease across the life span. Nat Med. 2019 Dec;25(12):1822–32.
9. Hsu TW, Bai YM, Tsai SJ, Chen TJ, Chen MH, Liang CS. Risk of autoimmune diseases after post-traumatic stress disorder: a nationwide cohort study. Eur Arch Psychiatry Clin Neurosci. 2024 Apr 1;274(3):487–95.
10. Mandagere K, Stoy S, Hammerle N, Zapata I, Brooks B. Systematic review and meta-analysis of post-traumatic stress disorder as a risk factor for multiple autoimmune diseases. Front Psychiatry [Internet]. 2025 Feb 20 [cited 2025 July 15];16. Available from: https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2025.1523994/full
11. Stojanovich L, Marisavljevich D. Stress as a trigger of autoimmune disease. Autoimmunity Reviews. 2008 Jan 1;7(3):209–13.
12. Agorastos A, Chrousos GP. The neuroendocrinology of stress: the stress-related continuum of chronic disease development. Mol Psychiatry. 2022 Jan;27(1):502–13.
13. Butjosa A, Gómez-Benito J, Myin-Germeys I, Barajas A, Baños I, Usall J, et al. Development and validation of the Questionnaire of Stressful Life Events (QSLE). Journal of Psychiatric Research. 2017 Dec 1;95:213–23.
14. Roohafza H, Ramezani M, Sadeghi M, Shahnam M, Zolfagari B, Sarafzadegan N. Development and validation of the stressful life event questionnaire. Int J Public Health. 2011 Aug 1;56(4):441–8.
About Dr Sula Windgassen, PhD
Dr Sula is a Health Psychologist, Cognitive Behavioural Therapist, Eye Movement Desensitisation & Reprocessing (EMDR) Therapist and Mindfulness Teacher. Trained at King's College London & publishing papers on the use of psychology to improve health and whole-person wellbeing.
Featured links
Copyright © 2026